ANTERIOR CRUCIATE LIGAMENT 2
-->
Treatment
- non surgical
- in those who are willing to make life style changes – avoid the activities of recurrent instability
- in cases of stable knee
- muscle strengthening – braces
- risk of meniscal tears high
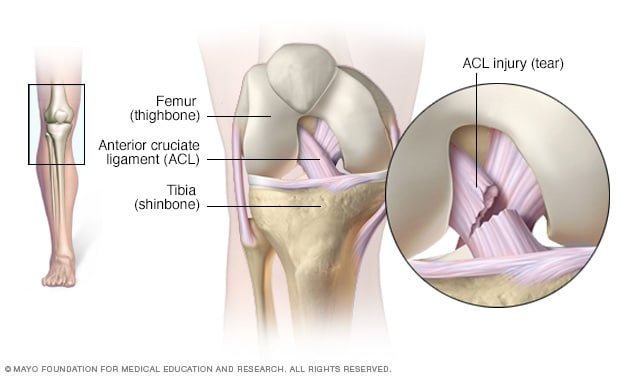
- repair of ACL
- 50% failure within 5 years
- primary repair indicated only in bony avulsion of ACL
- more tibial avulsions than femoral ( except skiers with low velocity injuries)
- avulsed bony fragment replaced, fixed sutures through trans osseous drill holes/screws
- post op 3 wks – up to 900 flexion allowed in brace – 6 wks crutches – 8wks full range motion- 3 months exercises continued
- reconstruction of ACL
- Extra articular
- intra articular
Extra articular procedures
- create a restraining band on lateral knee – from lat femoral epicondyle to gerdy tubercle – line parallel with ACL
- use iliotibial band
- stress depends on the changes of femoral fixation points – so transfer should be anchored high on femur – proximal to attachment of LCL
- decreases the anterolateral rotatory subluxation – do not recreate normal anatomy – high chance of failure when used alone
- used along with intra articular reconstruction
- Techniques
- Macintosh technique (iliotibial band tenodesis)
- 1.5 cm band strip dissected from mid portion – at 16 cm from distal insertion – passed through hiatus created in distal inter muscular septum – passed deep to fibular collateral ligament – fixed to gerdy tubercle with staples or sutures
- Losee modification of Macintosh technique
- 18cm long, 1.5 cm wide strip of iliotibial band – distally attached to gerdy tubercle – passed through an osseous tunnel created in anterolateral femoral condyle – through the femoral attachment of lateral inter muscular septum and lateral head of gastrocnemius – fixed to gerdy tubercle with suture/ staple
- Andrew's technique
- anterolateral 10cm hockey stick incision exposing iliotibial tract
- longitudinal division of tract – 10cml long at 4 cm anterior to posterior margin of tract
- separated into two bundles – fixed to femur by sutures – passed through tract – through 2 parallel holes to distal femur – fixed to each other at medial side of femur beneath vastus medialis
- anterior bundle tight in flexion – posterior bundle tight in extension
Intra articular reconstruction
- arthroscopically or small arthrotomy incision
- Graft selection
- autografts – allografts – synthetic grafts
- autografts – low risk of inflammation – no risk of disease transmission
- most common choices
- bone - patellar tendon -bone graft
- 8-11mm wide
- central third patellar tendon with adjacent patellar and tibial bone block
- strength – 2977 N
- quadrupled tendon graft
- quadruple stranded semitendinosus graft or quadruple stranded semitendinosus – gracilis tendon graft
- quadriceps tendon graft
- harvested with patellar bone or entirely soft tissue graft
- ACL strength – 1750 N - strength of graft decreases to half when fully taken up – so initial strength of graft should be 2x1750 N
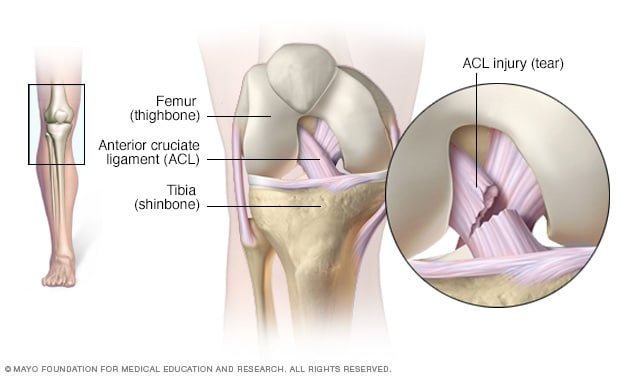
- Graft placement
- femoral site more important – closer to the center of axis of knee motion
- femoral tunnel – too anterior – intra articular distance lengthens in flexion – leads to knee capturing or loss of flexion – failure of graft
- posterior placement of tunnel – graft taut in extension and lax in flexion – produces an acceptable result – ACL cause knee stability is in the end of extension – clinical examination negative Lachman and Ant drawer but posterior drawer +
- isometric placement of tunnel is preferred location – that limits changes in length and tension in movement
- posterior portion of ACL tibial insertion near the posterolateral bundle location – best reproduction of intact ACL function – decreases graft impingement against roof of intercondylar notch in extension ( as in an anterior placement)
- tibial bone plug – triangular – patellar - trapezoidal
- Notch plasty – widening of the intercondylar notch – prevent impingement – posterior tibial placement requires minimal notch plasty
- needed in c/c ACL deficiencies, intercondylar notch stenotic w/ osteophytes
- limited notch plasty improves visualization – assist in proper placement of tunnel
- anterior aspect of notch deepened by 2-3cm – depends on size of graft
- tapered posteriorly – so no bone is removed at femoral insertional site
- bony ridge / resident's ridge – anterior to femoral attachment of ACL removed – hinders proper identification and placement of tunnel
- posterosuperior apex of the notch at 12'o' clock – funnel canal should be at 11'o'clock in right knee and at 1'o'clock in left knee
- Graft tension
- that much needed to obliterate Lachman test
- less tendon needed for b-pt-b graft than semitendinosus graft – tendon portion in b-pt-b is short and stiffer
- Graft fixation
- early post op – weak ling is fixator not graft tissue
- direct fixation – interference screws, staples, washers, cross pins
- indirect fixation – polyester tape – titanium button, suture
- interference screws popular for b-pt-b graft
- complications are
- inadvertent graft advancement unless graft fixed correctly while inserting the screw
- screw laceration of passing suture – place at least one suture on opposite side of bone plug ( side which has no contact with screw threads)
- screw thread laceration of tendon – if tip protrudes out of bone
- screws parallel to bone plug and tunnel wall – ensured by using cannulated screw system
- bioabsorbable screws – good alternative to metal screws
- bone to bone healing in b-pt-b graft is 6 wk – bone to tendon is 8-12 wks – rehab during this period gives additional stress of 450N – this period fixation strength determines the failure – once graft taken up graft strength limits failure
Order Books Videos Notes and study material shop.orthodnb.com
Orthopaedics made simple for DNB MS MRCS Support and Guidance for DNB Orthopaedics, MS Orthopaedics and Orthopaedic Surgeons. DNB Ortho MS Ortho MRCS Exam Guide Diplomate of National Board.Our site has been helping dnb ortho post graduates since a long time.It has been providing the dnb ortho theory question papers,dnb orthopedics solved question bank, davangere orthopaedic notes, sion orthopedic notes.We provide guidance to post graduates as to how to pass dnb and ms ortho exams, and aspiring orthopaedic surgeons surgical technique teaching videos and orthopaedic books and pdf.
Get updates email orthoguidance@gmail.com whatsapp 9087747888
- Study Material to Pass Any Orthopaedics Exam
- Davangere Orthopaedic notes pdf
- Dawangere Ortho Notes Hard copy all volumes 2017 edition
- DNB Solved Question Bank with Answers
- Ortho Theory Exam Package
- Ortho Practical exam package
- Ortho case presentation videos
- Orthopaedic Journals
- Orthopaedic Physical Examination video Atlas
- Sion Hospital Orthopaedic Notes
- Orthopaedics Proformas and scheme of practical examination
- Orthopaedic instruments videos and extras
- Video Atlas of Human Anatomy
- Ortho Practical Exam Guide
- MRCS Package
- Orthopaedic Surgery Technique teaching videos - Trauma
- Orthopaedic Surgery Technique teaching videos - Arthroplasty
- Orthopaedic Surgery Technique teaching videos - Spine
- Orthopaedic Surgery Technique teaching videos - Shoulder Arthroscopy
- Orthopaedic Surgery Technique teaching videos - Knee Arthroscopy
- Anatomical Approach technique and exposure teaching videos
- Orthopaedic PG Course Videos










It is pleasantly demonstrated. Spinal line harm leads to walking inability. The individual needs steady to move from one put to another. A lightweight wheelchair can do that from times to times. There is numerous diverse sort of wheelchair that can be profit depending on client comfortably. Wheelchair accessories
ReplyDelete